 I was recently called to attend to a 55yr old female patient complaining of “Chest Pain”
I was recently called to attend to a 55yr old female patient complaining of “Chest Pain”
On arriving on scene I was shown to an upstairs bedroom where the patient was sitting on the edge of the bed. Fully conscious, alert and orientated. Good colour, no sweating, not short of breath and apparently in good spirits.
History taking revealed a 6 hour history of epigastric pain (i.e. just below the bottom edge of the sternum) which eased slightly about 4 hours ago then came back with a vengeance approximately 2 hours ago. The patient wasnt the best historian and the only description I could get for the pain was that it was like “an indigestion type pain”.
I asked her if she suffers with indigestion to which she replied:
“No, I dont have any health problems and have never had indigestion”
Which begs the question, how can she describe it like and indigestion pain if she has never had indigestion? I delve a little further into her pain following the usual pain assessment:
Nature: Still describes it as indigestion. She doesn’t say any of the magic words – Crushing, Tight, Ache, etc
Severity: Really bad. Cannot give a pain score figure, but just says its really bad.
Duration: As above, however, the exact time that the pain got worse seems to be varying each time its mentioned.
Location and Radiation: Definitely epigastric, denies any sub sternal or central chest pain, however pain is radiating to her left axilla.
Exacerbation: Not worsened by movement, deep inspiration, palpation or coughing.
Relief: She has not gained any relief from resting but does feel a little better since I arrived (the amazing effect of the green jumpsuit!!)
As we are talking, she is also gulping down mouthful’s of air and belching loudly. My thoughts are turning towards pain from a gastric origin, but things aren’t clear cut here, not be a long way.
Out comes the Lifepak 12 for a 12 Lead ECG. I explain what I am doing and that it is all just routine because she is saying that she is having chest pain, even though it appears gastric.
“Lets just do the test so that we can put that out of your mind and move on to what is causing this pain”
I watch the ECG roll print out. Limb leads look fine. Anterior leads…….You’ve got to be kidding me!!
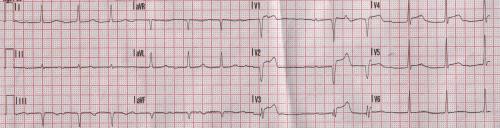
The 12 Lead shows that she is having a significant anterior MI (heart attack).
I wasn’t expecting that!
Time for a quick change in focus and drive. By now the crew have arrived and I have given them a very quick handover and then talk to the receiving PPCI (angioplasty) suite. They are initially skeptical about taking her as she has not said any of the magic words and looks “well” in herself. Initially, the nurse that I was discussing the case with thought that the ST segments looked a bit “saddle-bag” like (a signifier of pericarditis rather than an MI) and seemed a little reluctant to call the team in from home as the presentation was so atypical. I stop and have a look at the ECG again, and I really think that this looks nothing like a pericarditis, there is no wide spread ST elevation, I feel that there is no saddlebag signs, no depressed PR segment and the patient does not present with pericarditic pain. The nurse agrees to accept the patient for PPCI and the call goes in to get the consultant in from home to do the procedure.
I explain everything to the patient and their family. They are obviously surprised (although I wonder if they were as surprised as I was?) but seem to handle the information well.
The crew now take over and I go back to my rapid response car to fill out the patient report form. As I am writing it, I reflect and think if I missed anything but I come to the conclusion that this was just a very atypical cardiac chest pain. I have had them before, but not where I would have put money on it not being a MI. The golden rule to take away from all of this is that not all cardiac pain is in the chest! Sounds a bit daft, but that is why a full assessment is required for any patient saying “chest pain”, even if they are saying or pointing to a different area (within obvious reason!)
At the end of the day, it made no difference what mine and the crews thoughts were. She still got the works, which gave us our diagnosis and the correct treatment plan.
I contacted the PPCI centre later in the shift to find out the results of the angio.
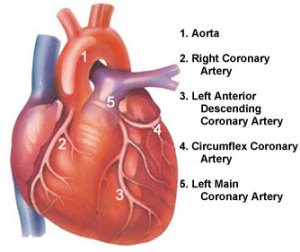 This showed a completed occlusion of the LAD (left anterior descending artery).
This showed a completed occlusion of the LAD (left anterior descending artery).
The patient was stented within 20 mins and blood flow returned to the myocardium, and is now doing well on the ward.
Job Done!










VERY nice one.
By: MarkUK on April 26, 2009
at 9:02 pm
Nice work.
I’ll bet you are glad she wasn’t having a NSTEMI or a NSTEACS
(non st segment elevation acute coronary syndrome)
(apparently the latest and greatest terminology).
Many others have left them at home (no ecg signs), only to re-repond an hour later to a cardiac arrest. Not good….
And if you or anyone else is interested, our pain questions are NILDOOCARRF (said nil doo carrf).
Nature
Intensity
Location
Duration
Onset
Offset
Concomitant factors
Aggravating factors
Relieving factors
Radiation
Frequency
Weird maybe, but it works for us (others in Australia use OPQRST)
Regards
Dave
By: Dave on April 27, 2009
at 10:48 am
Mark, That was very close but also very good nice to know your listening to that little voice in your head, well at least one of them!!
regards,
Eamonn
By: Eamonn on April 27, 2009
at 4:34 pm
Once you start “expecting” everything you can expect for your vision and thought processes to get clouded and prejudicial. You’ll start looking for what you expect and could miss what you DIDN’T miss this time.
Good call!
By: Beverly, RN on April 29, 2009
at 11:17 am
Excellent example – women are alarmingly dismissed or misdiagnosed when having cardiac events! Research in the past decade has revealed many differences in how women present with cardiovascular symptoms.
I am a heart attack survivor and a 2008 graduate of the ‘WomenHeart Science & Leadership Symposium for Women With Heart Disease’ at Mayo Clinic in Rochester, Minnesota last fall.
Please visit ‘Heart Sisters’, my website at http://www.myheartsisters.org – devoted exclusively to the subject of women and heart disease. I’d appreciate your feedback.
Many thanks,
Carolyn Thomas
By: Carolyn on May 3, 2009
at 5:50 am